By James Clark, Steven R. Goldring, John Norton Moore, Daniel J. Pambianco, and Guy B. Roberts
Greater pandemic preparedness will require improvements in infrastructure, early warning, testing, contact tracing, enhanced communication, and international cooperation, as detailed by a recent independent task force report of the Council on Foreign Relations. But simply doing better in these defensive areas of pandemic response is not sufficient for the level of threat we face. Over the last year, scientists have massively expanded our understanding of viral biology and targets for drugs and vaccines, and several members of the task force called for a “public-private partnership to take corona viruses and influenza viruses off the table as future pandemic threats.” A massive program to attack these viruses is essential for our future national security and economic well-being.
Covid-19 has already imposed a horrendous economic cost on our country, but a new pandemic poses a catastrophically greater threat. Another pandemic sparked by a new corona or influenza virus or a mutation to the Covid-19 virus resistant to existing vaccines would heap economic devastation on top of that already incurred by Covid-19.
And it is not just the reappearance of corona and influenza viruses and their mutations we need to fear; the demonstrated vulnerability of America and our allies to the Covid-19 virus has given impetus to bio-terror attacks. Obtaining weapons-grade plutonium or Uranium 235 to make nuclear weapons has proven difficult for terrorist actors, but revolutionary and readily available new genetics technologies make it continually easier to access and deploy bio-weapons.
For too long, we have accepted tens of thousands of influenza deaths each year, in some seasons exceeding the number of traffic deaths. Because influenza mutates rapidly, vaccine makers must make educated guesses each year about what strains to cover, sometimes resulting in vaccines with little protective value. Covid-19 is novel and far more deadly than existing influenza viruses, and it is constantly mutating to be more infectious and, in some cases, more lethal. The likely reality is that Covid-19 in some form is here to stay. How many lives will it continue to take, even after widespread distribution of extant vaccines?
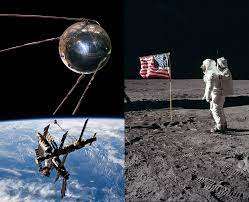 Given the frequency at which new corona and influenza viruses are now appearing in a world ever more conducive to viral spread, we must put in place a major national program for pandemic preparedness akin to the Apollo Project. That effort which took Americans to the moon for the first time cost approximately $25.4 billion in 2019 dollars — a trivial amount in comparison with the trillions of dollars the Covid-19 pandemic has already cost us.
Given the frequency at which new corona and influenza viruses are now appearing in a world ever more conducive to viral spread, we must put in place a major national program for pandemic preparedness akin to the Apollo Project. That effort which took Americans to the moon for the first time cost approximately $25.4 billion in 2019 dollars — a trivial amount in comparison with the trillions of dollars the Covid-19 pandemic has already cost us.
A national program should be a public-private partnership drawing on both government expertise and that of the private sector. It should seek to improve all the traditional, defensive measures of pandemic response such as early warning, testing, tracing, and vaccine financing and delivery. But it should also seek to decisively defeat corona and influenza viruses through a full research attack against the biology of these viruses and their effects on their human hosts.
Ongoing advances in viral biology, more effective antivirals including monoclonal antibodies, and improved vaccine development suggest that it is a reasonable goal to eliminate the risk posed by corona viruses and influenza viruses. Covid-19 has already prompted an extraordinary pivot in biological and medical research. Focused and well-funded efforts are needed now on more efficacious antivirals, including efforts focused on essential properties of virus infection, replication, and organ damage, as well as development of new vaccine technologies to generate effective and lasting immunity.
Present approaches for viral infection are based on vaccines that prime the immune system to prevent viral entry into host cells, but there is a need for additional therapies that inhibit viral replication, transmission and tissue injury. In addition, more effective therapies need to be developed to prevent lung damage and respiratory distress that accompany viral infection.
 Existing technologies need to be used to develop more effective antiviral therapies, including high throughput screening, reformulation and modification of existing antivirals, and further evaluation of novel therapies, including the use of convalescent plasma, monoclonal antibody therapy, and inflammatory modulators that target pro-inflammatory mediators and cytokines. Further, we need to apply new technologies in the search for more effective antiviral therapies, including computer-aided design, nanotechnology-based drug delivery platforms, and combinatorial nanotechnology-based treatments. More rapid, sensitive and specific diagnostic tests also are needed. We need to expand research into the cellular and molecular mechanisms that regulate host responses to viral pathogens and the application of genomic and related molecular biological technologies to identify the role of individual host factors in the risk for viral infection, dissemination and disease severity.
Existing technologies need to be used to develop more effective antiviral therapies, including high throughput screening, reformulation and modification of existing antivirals, and further evaluation of novel therapies, including the use of convalescent plasma, monoclonal antibody therapy, and inflammatory modulators that target pro-inflammatory mediators and cytokines. Further, we need to apply new technologies in the search for more effective antiviral therapies, including computer-aided design, nanotechnology-based drug delivery platforms, and combinatorial nanotechnology-based treatments. More rapid, sensitive and specific diagnostic tests also are needed. We need to expand research into the cellular and molecular mechanisms that regulate host responses to viral pathogens and the application of genomic and related molecular biological technologies to identify the role of individual host factors in the risk for viral infection, dissemination and disease severity.
Developing effective vaccines is just the first step in distributing them to the population at large, which will require programs and strategies for earning the trust of individuals in both the public and the health care workforce and for increasing vaccination rates among minority racial and ethnic groups. Governmental regulatory agencies such as the U.S. Food and Drug Administration must have the resources and infrastructure to provide rapid and rigorous evaluation of new antiviral therapeutics and the Centers for Disease Control and Prevention should be empowered to conduct scientific evaluation and provide healthcare information in response to national health threats. In light of the global spread of the virus and its mutations, efforts to curb the pandemic and to distribute vaccines and antiviral therapies need to be coordinated at both the national and international level.
Given what Covid-19 has taught us about the catastrophic costs of being unprepared for a viral pandemic, we must put in place effective defensive approaches to pandemic preparedness — but we must take the fight to the biology of the viruses and their host responses themselves.
Dr. Steven R. Goldring, MD, is the former Richard L. Menschel Research Chair, and Chief Scientific Officer, of the Hospital for Special Surgery in New York and a former Professor of Medicine at Harvard; John Norton Moore is a Professor of Law Emeritus at the University of Virginia and a former Chairman of the American Bar Association Standing Committee on National Security Law; Guy B. Roberts is former Assistant Secretary of Defense for Nuclear, Chemical, and Biological Defense Programs and former Deputy Secretary General at NATO for Weapons of Mass Destruction Defense , and Dr. James Clark, MD, and Dr. Daniel J. Pambianco, MD, are practicing physicians with extensive experience in medical research and human trials.

